Infraoccluded teeth as bone anchors for the resolution of tooth impaction and for maxillary protraction
Published: June 2012
Bulletin #12 – June 2012
Infraoccluded teeth as bone anchors for the resolution of tooth impaction and for maxillary protraction
Infraoccluded teeth cannot be moved by orthodontic forces. It is therefore logical to use them as a base from which to apply orthodontic forces to other teeth, in the same way as TAD’s are employed. Equally, maxillary infraoccluded teeth may be used as bone anchors for the application of orthopedic forces to the entire hypoplastic maxillary skeletal complex in a skeletal class 3 case.
The following case report is an example of where both these principles were employed in a patient with multiple congenitally missing teeth, including solitary mandibular molars bilaterally impacted in the anterior portion of the vertical ramus.
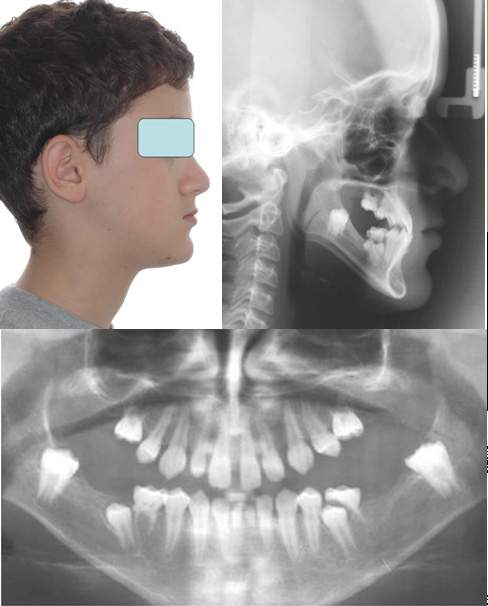
Fig. 1 Initial pre-treatment views of the patient, clinically and radiographically in profile and the panoramic view to show the large number of missing teeth. All four deciduous second molars were present, together with the mandibular deciduous central incisors. The unerupted isolated molar on each side was impacted in the junction between the body and vertical ramus of the mandible.
The patient
was first seen in the Department of Orthodontics of the Hebrew
University-Hadassah School of Dental Medicine in November 2006, when the
initial records were made (Fig. 1). He was a 12 year old male with a flat
facial profile lacking malar eminences, a mild skeletal class 3 relationship,
due to maxillary hypoplasia and mildly overclosed appearance. The erupted teeth of his permanent dentition were very small and the only ones
present in the upper jaw were the widely spaced four incisors, the canines and
the first premolars. Distal to the first premolars was a
solitary severely infraoccluded second deciduous molar on each side. In the
mandible, the lateral incisors, canines and first premolars were present,
together with deciduous second molars and two deciduous central incisors (Fig.
2). The radiographs revealed unerupted mandibular second premolars abnormally
related to their deciduous molar predecessors and a single unerupted permanent
molar on each side, impacted in the anterior part of the vertical ramus.
Fourteen permanent teeth were congenitally absent, in a symmetrically bilateral
manner, in each jaw.
Fig. 2 The intraoral views of the dentition show the initial degree of infraocclusion of the deciduous molars and the secondary effect that the more severely affected maxillary molars had on the teeth premolars and canines1. The occlusion was delicately balanced on 3 incisor and right canine contacts only.
The problem list included a flat facial profile, an under-developed maxilla, a very broad lateral open bite with no posterior occlusion, anterior crossbite, small teeth, spaced teeth, missing posterior teeth, missing lower central incisors, retained and loose deciduous lower central incisors, infraoccluded maxillary deciduous molars and bilaterally symmetrical solitary mandibular molars impacted in the vertical ramus.
Orthodontic redistribution of the relatively few teeth in each dental quadrant was essential, if the eventual prosthodontic rehabilitation would stand a good chance of producing a successful outcome.
Treatment timing
While prosthodontic treatment would obviously be necessary in the long term to rehabilitate the many missing units in the dentition, this could not be considered for another 10 years or so, because of the child’s age. In the meantime, therefore, some form of temporary rehabilitation would need to be undertaken for the period during the orthodontic treatment, once the lower deciduous central incisors were lost. Provisional prosthodontics would also need to be combined with the retention regimen at the completion of the orthodontic treatment.
From the restorative point of view, it would be most advantageous to undertake the orthodontics immediately prior to the time for the preparation and placement of the definitive prosthodontic units, so that the interface between the two specialties could be as seamless as possible.
From the orthopedic/skeletal point of view and with the child approaching adolescence, there was no time to be lost if maxillary protraction was to have its greatest effect. Socially among his peers, too, the acceptability of his wearing a protraction face mask for sufficient hours in the day was already in serious decline. From the orthodontic standpoint, the time was about right, with only 2 remaining mandibular deciduous molars that had succedaneous premolar teeth beneath them, which were of sufficiently advanced root development for them to be included into the erupted dentition.
The rationale for beginning treatment at this age was preferred, since it offered the greatest potential for differential skeletal growth in favor of the maxilla without the need for surgery, which the parents had refused. However, it was recognized that a long period of retention combined with temporary prosthodontic rehabilitation would be required between the completion of the orthodontic treatment and the commencement of prosthodontic oral rehabilitation.
Treatment plan
The following is a treatment priority list that was adopted for this patient:-
- protraction of the maxillary complex, using the infraoccluded deciduous second molars as the site of force application.
- aligning the erupted teeth in the mandibular dentition and creating space for eventual prosthodontic rehabilitation of the missing permanent central incisors.
- permitting the mandibular second premolars to continue to erupt distal to their infraoccluded deciduous predecessors, so that the latter may eventually be exploited for their anchorage value in moving other teeth, before they are finally extracted.
- surgically exposing and bonding attachments to the two permanent molars in the anterior vertical ramus, in a closed exposure procedure.
- placing a screw TAD in the left premolar region of the mandible for anchorage
- using the infraoccluded right deciduous second molar as an anchor tooth.
- when the deciduous mandibular central incisor would be shed naturally, temporary prosthodontic replacement would be necessary
- drawing the molars mesially against the left TAD and the right infraoccluded deciduous molar.
- aligning and closing spaces mesially in the maxilla and creating a normal overjet and deepening the overbite.
- retention until definitive prosthodontic treatment can be initiated, to include implants, crowns and fixed prosthodontic restorations.
This treatment plan was coordinated with the prosthodontist from the outset and reviewed at certain stages in line with the progress of the treatment. .

Fig. 3a Buttons were bonded buccally and lingually on the infraoccluded deciduous molars
Fig. 3b The customized face mask in place
Fig. 3c Elastic traction may be applied from the buccal button, as shown here, from the lingual button or from both, to protract the maxilla.
Treatment
A custom-made clear plastic face mask was constructed for this patient, using a cast plaster model of the face (Fig. 3).
The impression for this plaster model was made using a plaster-impregnated bandage, more commonly used in orthopedic clinical practice for the fabrication of a plaster cast to splint a broken limb. In preparation for the impression, a broad sheet of thin plastic film was stretched around the patient’s head – taking care to leave a cut area over the mouth through which the child could breathe!! The most suitable material is thin plastic “cling foil” which is used to cover dishes containing salads and other prepared foods before being placed on the table and which is available on a wide roll in any home store.
The patient lay horizontally in the dental chair while the water-saturated plaster bandage was placed round and round in several circular layers around the face, from the hairline, via the cheeks on each side, over the upper lip and down to include the full contour of the chin. It was left in place until the child noticed that the plaster became warm, indicating that the plaster had set, through its exothermic chemical reaction. The plastic “cling foil” was then freed initially from the back of the head and carefully pealed forward off the face, without separating it from the set plaster impression. It is emphasized that this procedure should never be done directly on the face, since its removal will be extremely painful, with the fine hair of the face becoming trapped in the set plaster – even in girls and pre-pubertal boys.
The “death mask” was now transferred to the lab, where the technician poured a model directly over the plastic covered impression surface. The presence of the “cling foil” greatly facilitated the subsequent separation of the model. If the plastic peels off during the removal of the impression from the patient’s face, then a separating medium will need to be applied to its surface before pouring the model.
The face mask was constructed of clear acrylic pad on the forehead and on the chin, which were linked through a wire frame ringing the lateral aspects of the face. A soldered wire cross piece stood a few millimeters clear of the front of the mouth, with two soldered hooks for the placement of the protraction elastics.
Commercially available face masks are obtainable from most of the supply companies, with prepared “one-size-fits-all” chin and forehead pads, which fit everyone because of the thick felt padding and fit nobody without it. The pads, therefore, have to be colored, and thick, if they are to be comfortable. They may be supported by a vertical middle-of-the-face bar with adjustable height cross piece for the application of rubber bands. Other types of face mask exist, but the pads remain the same. As the result, these appliances are very obvious and clumsy, with even the best patient relegating it to being worn only very few of the hours of the day.
Nobody likes to wear a face mask! Nonetheless and in direct contrast to the commercially made alternatives, the custom-made clear plastic pads fit the chin and forehead very well. It requires no padding and are thus less visible. As the result, the appliance is much thinner with more modest and simple lines and much less obvious. It is much more user-friendly and patients are prepared to wear them for many more hours, including during the day and often (with a little encouragement) even during school.
In the present case, lingual and buccal buttons were bonded to the deciduous second molars in the maxilla (Fig. 3a) and elastic protraction mechanics were applied from them to the hooks on the cross piece of the face mask (Fig. 3c). The patient was asked to wear the appliance full time and, initially he followed this regimen. In later months, his enthusiasm lagged and parental influence lessened, as he approached and passed puberty, largely for understandable social and psychological reasons. Nevertheless, a good degree of skeletal improvement had occurred within 12 months of treatment (Fig. 4).

Fig. 4. Following a year of maxillary protraction, with ups and downs in patient cooperation, there was much improvement in the skeletal relationship. A positive and significant anterior overjet had established, the overbite had deepened due to occlusal contacts with the lateral incisors and canine and the formerly proclined maxillary central incisors had become markedly retroclined.
The teeth in the mandibular arch were aligned and leveled with a fixed Tip-Edge set-up and additional space was provided in the area of the deciduous central incisors, in preparation for their replacement with normally sized artificial teeth.
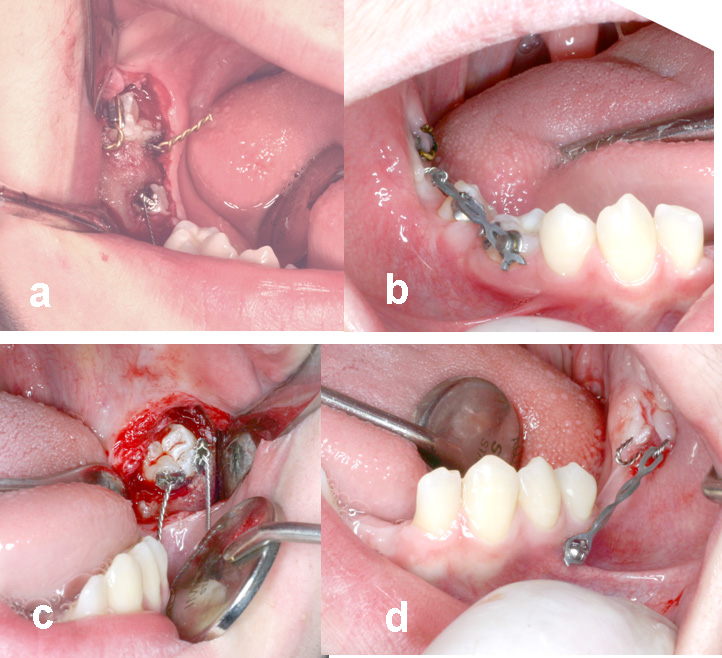
Fig. 5 a, b. On the right side, the unerupted molar and second premolar were exposed and attachments placed on each. The infraoccluded deciduous second molar was left in place. Because of the depth of the tooth within the mobile soft tissue covering the ramus, only a closed exposure was possible. Traction was applied 3 months later from one of the twisted ligature attachments on the molar to a button placed on the infraoccluded deciduous molar, aimed at tipping the impacted tooth out of the soft tissue.
Fig. 5c, d. A similar procedure was carried out on the left side except that the deciduous molar exfoliated naturally and traction was made to a screw TAD, on the same day.
Twenty months later, the solitary molars were exposed (Fig. 5) and two small eyelets bonded to each of them with brass wire ligatures fashioned into small traction hooks ligated into them. The surgical flaps were then fully replaced in a closed exposure procedure, leaving only the brass hook visible emanating through the sutured edges of the flaps. Traction was applied initially to generate a mesial tipping movement, in order to erupt the two teeth mesially through the mucosa in the retromolar area.
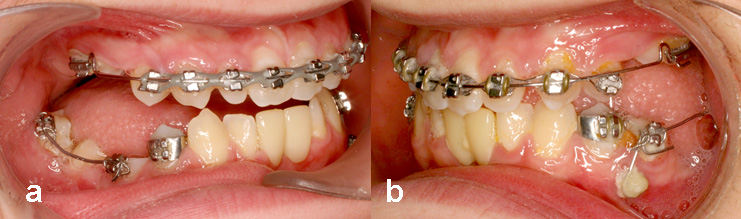
Fig. 6. two artificial acrylic teeth replaced the exfoliated deciduous incisors and were held in place by a lingual arch soldered to orthodontic bands on the first premolars. In the maxillary arch, the spaces were closed by moving all the teeth mesially, to establish normal axial inclination of the incisors and a normal overbite and overjet.
- A simple cantilever spring was inserted into the molar tube at one end and was raised and ligated into a bracket on the infraoccluded molar, at the other end. Both ends were cinched and, because the deciduous molar represents a form of absolute anchorage, the full deflection of the spring caused a mesial uprighting of the roots of the permanent molar.
- On the left side, a similar uprighting mechanism was used between the tipped permanent molar and the erupted second premolar. In order to reinforce the anchorage of the latter, a rigid wire connection linked the premolar bracket with the TAD, using composite adhesive.
Further
mesial movement was combined with mesial root movement of the molars to achieve
good uprighting, relying heavily on the attachment
on the infraoccluded molar on the right (Fig. 6a) and on a TAD on the left side (Fig. 6b). During this
period, the deciduous central incisors were shed and a lingual arch carrying 2
artificial incisors, soldered to first premolar bands, was cemented into place. 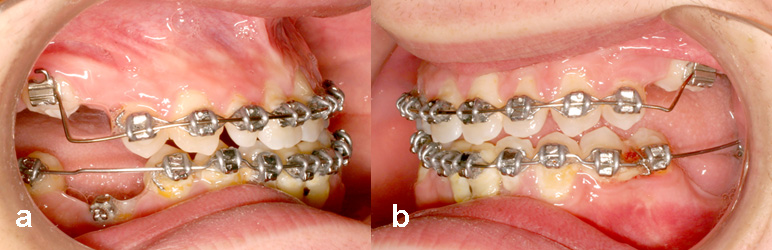
Fig. 7. The height differential between the 3 remaining infraoccluded deciduous molars and the erupted and aligned permanent teeth illustrates how much vertical growth had occurred since the beginning of treatment and how much the secondarily infraoccluded premolars and canines had been extruded into occlusion.
A full arch Tip-Edge strap-up was placed in the maxillary arch, offset at the infraoccluded deciduous molars, to compensate for the extreme height difference of these teeth to the permanent teeth (Fig. 7). The spaces between the permanent teeth in the maxilla were closed, the teeth aligned by mesial movement with the use of expanded coil springs, a more normal incisor relationship was achieved and the lateral open bite was closed.

Fig. 8 a-c. The intra-oral photographs of the dentition on the day appliances were removed. Note that the mandibular right second premolar had been erupted into close proximity to the fully uprighted molar on that side. The two molars were excellent potential abutment teeth for future reconstruction. Oral rehabilitation of the missing mandibular incisors and the posterior teeth in both jaws will be compromised by the relative lack of height of the alveolar ridge and its narrow knife-edge appearance.
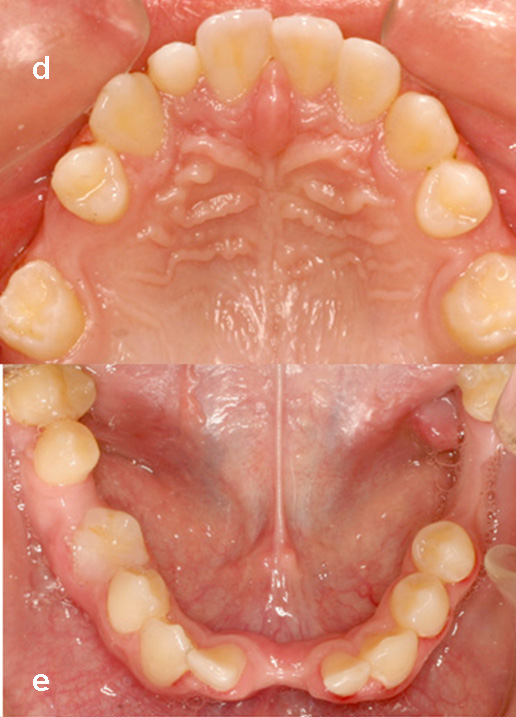
Fig. 8d, e. The occlusal views of the dentition.
The clinical photos taken on the day of debonding (Fig. 8a-e) show considerable improvement in the inter-arch relation that occurred due to the maxillary protraction. At the same time, they illustrate the excellent bodily mesial movement of the previously impacted mandibular molars, over a very considerable distance. These teeth now assume strategic importance as potential abutments in the future planning of the prosthodontic reconstruction of the dentition as a whole.

Fig. 9a. The panoramic view shows the 3 remaining infraoccluded deciduous second molars. The mandibular right second molar is adjacent to the molar and the molar teeth have been moved well clear of the vertical ramus.
Fig. 9b. The lateral cephalogram at the completion of treatment.

Fig. 10. Superimposition of the pre-treatment (black lines) and post-treatment (red lines) cephalogram tracings illustrates the degree of protraction of the maxilla and very considerable bodily mesial movement of the two mandibular molars (Courtesy of Yael & Eyal Katzhendler and Orthodata Co.). The skeletal relations and soft tissue facial profile are much improved.
The post-treatment panoramic and cephalometric views (Fig. 9), taken on the same day, show the new alignment and relationships of the teeth and jaws and the distancing of the mandibular molars from the ramus. The superimposed tracings from the pre-treatment and post-treatment cephalograms (Fig. 10) offer a quantification of the changes achieved. The patient's profile before and after treatment is presented here for comparison (Fig. 11).

Fig. 11. The patient’s facial profile pre- and post-treatment.
Retention
It will be appreciated that when changes in tooth shape and rehabilitating missing teeth are planned as the next phase of treatment, the retention of the treated result must also be carefully planned in cooperation with the prosthodontist concerned and it will need to be re-evaluated at every stage, when any change is made in the dentition. The alignment of teeth and the alteration of spaces will suffer significant relapse even after hours and certainly days, when the movement of the teeth is not carefully controlled. A simple suck-down Omnivac type of plastic overlay is easy, quick and cheap to make and is a great asset in these cases.
At age 15 years, the patient was debonded and Omnivac retainers were placed. The patient was referred to the prosthodontist for re-evaluation and consideration of placing temporary artificial teeth in the mandibular incisor region, while still maintaining the overall alignment of the other teeth in both jaws.
Reference
1. Becker, A. and Karnei-R'em R.M.: The effects of infraocclusion: part 2 - the type of movement of the adjacent teeth and their vertical development. American Journal of Orthodontics 102:302-309,1992
Postscript and apology
In the approach to treatment used in this case, orthodontists who survive the rough and tumble of daily clinical practice will recognize the potential for ups and downs in the patient’s attitude, mood changes and, as the result, compliance level. This reflects crucially on our ability to achieve a good outcome when we need to encourage, bludgeon and bribe the patient to wear the dreaded face mask for enough hours during the long months of treatment and to maintain the much needed oral hygiene. In this case report, the discriminating reader will see evidence of these shortcomings and the fact that appliances were removed prematurely, against professional advice and at the insistence of patient and family – for which the writer craves indulgence and begs forgiveness! Notwithstanding, the writer takes the liberty of presenting the incomplete case records for the lessons it conveys.
Reader feedback: I wish to recognize and thank Dr. John Kanyusik of Minnesota for pointing out a significant genetic association between severe forms of oligodontia and colon and ovarian cancer.
* Oligodontia: defined as six or more congenitally missing permanent teeth, third molars excluded
* Lammi, et al. Mutations in AXIN2 cause familial tooth agenesis and predispose to colorectal cancer. Am J Hum Genet 2004;74(5):1043-50
* Chalothorn, et al. Hypodontia as a risk marker for epithelial ovarian cancer. JADA, 2008;139:163-68
This is something about which we need to inform our affected patients and those involved in their medical care.



